Here we look at the facts on the vaccine – we speak to experts to find out more about its development, how it works and why it’s safe.

Here are helpful tips on how you and your loved ones can better cope with the pandemic and its effects.


Got the jab … Now what?
Are you now free to live your life as you did before the pandemic? We’ve compiled important information you should know before you head out into the world.
So, you just got your Covid-19 jab. Congratulations! Now, before you go mask free and hug family and friends, there are a few things you need to know.
When are you fully vaccinated?
All the Covid-19 vaccines are considered effective at protecting you from getting sick, and research from the US Centre for Disease Control and Prevention shows that people who are fully vaccinated can now safely do certain activities that they previously couldn’t due to the pandemic.
You are considered fully vaccinated if you meet these two requirements:
1. It has been two weeks after your second dose in a two-dose series.
2. It has been two weeks after your jab of a single-dose vaccine.
If you don’t meet these requirements, regardless of your age, you are not fully vaccinated.
What are the possible side effects after vaccination?
Reported side effects to the Covid-19 vaccines have mostly been mild to moderate and do not last long. More serious or long-lasting side effects to vaccines are possible but extremely rare.
Side effects are considered normal and indicate that your body is building protection. However, they may affect your ability to do daily activities.
The likelihood and severity of side effects differ depending on what type of Covid-19 vaccine you get.
The side effects include:
· fever
· fatigue
· headache
· muscle pain
· chills
· diarrhoea
· pain at the injection site
Severe reactions include a longer duration of the symptoms. They also include swollen glands or abscesses at the injection site that may result in hospitalisation, high and prolonged fever or collapse.
How to relieve side effects
Before taking any medication to relieve side effects, speak to your doctor about taking over-the-counter medicine.
Depending on the severity of your symptoms, your doctor might recommend medicine such as aspirin, ibuprofen, acetaminophen or antihistamines to help with any pain and discomfort.
If you have no other chronic illnesses, these medications may relieve post-vaccination side effects. It is, however, not recommended that these be taken before vaccination.
Side effects after your second jab may be more intense, but this is considered normal.
In the rare case that you get an allergic reaction to the Covid-19 vaccine, you need to seek immediate medical care. When you get the jab, you’ll be asked to wait at a designated area at the vaccination site for 15 to 30 minutes. Should you start to feel ill or have an allergic reaction during that time, there are medical staff on site who will help you.
Can you get COVID-19 after being vaccinated?
Yes. According to the National Institute for Communicable Disease, you may still be at risk of contracting Covid-19, but the disease will likely be milder in comparison to those who are unvaccinated. And it seems the vaccines are also effective against Covid-19 variants, such as the Delta variant.
More evidence is still required to confirm whether Covid-19 vaccines protect against asymptomatic or mild disease. More research is needed for ironclad confirmation, but it’s believed that those who are vaccinated are also less likely to spread the virus.
So, even if you’ve had the jab, you still need to wear your mask, practice social distancing and wash or sterilise your hands regularly. While you’re now less likely to contract the virus, and your symptoms will be much milder if you do, there are still groups – kids, people with certain allergies, women early in their pregnancy, etc. – who can’t get the vaccine and are still vulnerable.
EXTRA SOURCES: CDC.GOV; NICD.AC.ZA.

Going to or hosting a gathering? Here’s how you can stay safe from Covid-19
Larger get-togethers are allowed under level 1 lockdown, but that doesn’t mean you can let your guard down. Here are handy tips on how to protect yourself if you’re hosting a gathering or attending one.
Now that gatherings (limited to 750 people indoors and 2 000 outdoors) are allowed again, it’s tempting to just let loose and enjoy ourselves, but it doesn’t mean we should be lulled into a false sense of security.
Covid-19 is still all around. The death toll is rising daily, and new infections and hotspots are springing up all the time. Officials and experts have warned it’s more important than ever to be careful as lockdown fatigue deepens.
“Loneliness and isolation have had a terrible impact on mental health,” Cape Town-based psychologist Allengary Naicker says. “Many of us are longing to be with family and friends, but it’s important to consider each social event and what the potential risks are, especially for the elderly and those with comorbidities.
“We have to ask ourselves hard questions about what it means to take responsibility for our health and that of others.”
But that doesn’t mean you can’t have fun. It’s all about finding a balance where everyone is safe and comfortable.
As a host
The department of health (DOH) says every one of us could be exposed to the coronavirus at any time, so it’s imperative we take precautions.
Establish what your guests’ general Covid-19 safety protocols are before inviting them to your home. You wouldn’t want to risk catching the virus from someone who doesn’t share the same standard of adherence to the rules that you do.
The World Health Organisation (WHO) recommends including your home’s safety guidelines in the invitation and listing the extra precautions you’ll be taking for your event.
Some people could be asymptomatic or pre-symptomatic and not show any signs of being ill, the DOH warns. Ask prospective guests whether they’ve been exposed to the virus in the 14 days prior to your function. If they have – or even if they suspect they have – it’s best they don’t come.
Keep your numbers as low as possible – under 10 is best – to ensure guests can maintain the DOH’s recommended 1,5m to 2m distance from one another.
Remember, masks are the law. As a party favour you could prewash masks for the occasion and hand them to guests on arrival, along with small bottles of hand sanitiser, suggests US-based party company Wedgewood Weddings.
As a guest
Don’t attend any social function if you feel unwell or suspect you’ve been exposed to the virus, America’s Centres for Disease Control and Prevention (CDC) warns.
It’s okay – and you’re within your rights – to ask your host how many guests are expected to attend before you commit to going, Naicker says. If you’re uncomfortable being around too many people, it’s pointless joining the celebration as you’ll be too anxious to enjoy yourself.
Wear your mask when you’re not eating or drinking and wash or sanitise your hands frequently.
Safety first
Gathering outdoors is always preferable but if that’s not possible, ensure there’s good ventilation and seat guests about 2m apart.
Cape Town-based party planner Tara Eagles suggests using a bell or alarm set to ring every 30 minutes as a reminder for everyone to sanitise hands. “Ensure your guests don’t share glasses or cutlery. Make place settings and customised pegs for everyone’s glass,” she says.
“You could turn this into a fun activity for kids to do beforehand while familiarising them with your safety protocols. Make a sanitising roster for the day and allocate time slots to the older kids. Give them a ‘reward’ at the end of the event for their efforts.
“Lay out all the food on one table but let guests know it’s not a buffet. To avoid contamination while dining, nominate one or two people at most to dish up for everyone else. Ensure they’ve washed their hands thoroughly or even wear disposable gloves and they must wear masks while handling the food and utensils. Alternatively, guests could bring their own food for their household members.”
Guests should always wear masks except while eating or drinking. Keep a few unused masks at hand in case someone forgets theirs.
“And serve non-alcoholic drinks where possible to avoid reckless drunken behaviour – we all have that one uncle who parties a bit too hard,” Eagles says.
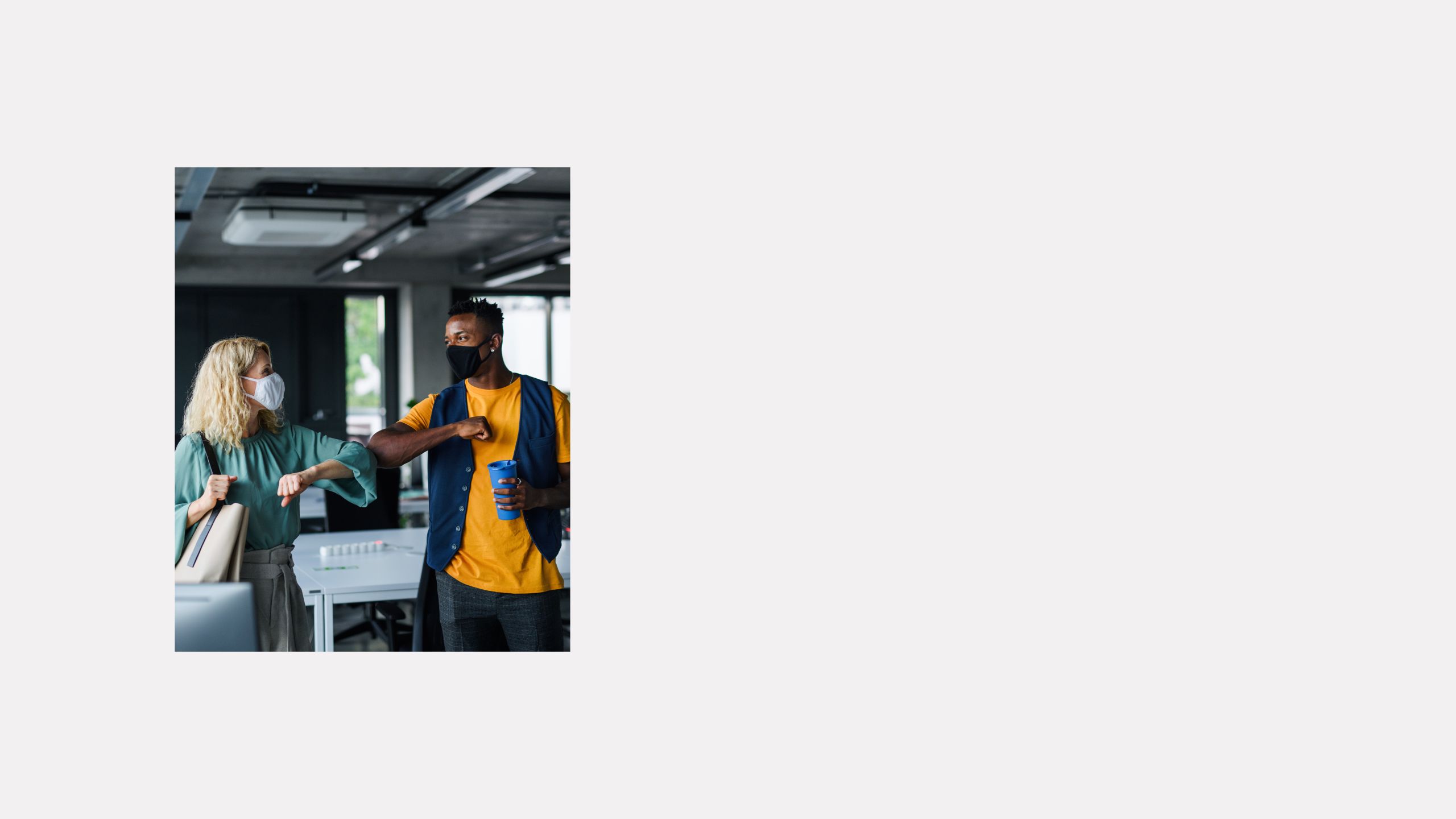
Let guests arrive and leave at staggered times to avoid crowding at the doorway, she adds. And remember to only use socially distant greetings such as elbow bumps or foot taps instead of hugging and kissing.
Make sanitiser easily available for frequent cleaning of hands and surfaces. Place hand sanitiser strategically near your front door and beside frequently used items and areas.
The toilet, bathroom sink, taps and door handles should be sanitised after each use – ask your guests to do this, Eagles says. Using an aerosol disinfectant spray on toilet and bathroom surfaces after washing your hands is a great way to keep these high-traffic areas safer.
Put single-use paper towels in the bathroom for guests to dry their hands on and leave a waste basket close by where they can discard their used towels.
How to say no
You don’t have to accept an invitation if you’re feeling uncomfortable in any way, Naicker says. Saying “I’m feeling so anxious that I think it’s best to stay at home” or “I’m worried about my mom or dad’s health, so we won’t be attending” are good ways to express your anxiety, she advises.
Don’t accept an invitation if you know you won’t be attending. Being a no-show breaks down trust in relationships.
“Saying no helps you establish healthy boundaries,” says Kissy Naude, a Cape Town-based life coach.
“Thank your host for the invitation but explain you’re still uncomfortable about socialising in a group. Honesty is the best policy.
“Tell your host you may be in a better position to attend a group engagement at a later date and that you’re always up for a virtual meeting,” she adds.
Giving back
If you decide to keep all your gatherings small – and it would be best to do so – consider donating food or money you might have spent on a fancy dinner or birthday party to help the less fortunate.
Contact your nearest food kitchen, children’s home or care facility for the elderly to find out how you can help.
To give a gift that keeps on giving, you could set up a monthly donation to a local or national feeding scheme. Some organisations to consider are The Lunchbox Fund, Food Forward SA, Siyabonga Africa in Gauteng and Ladles of Love in Cape Town.
How to help your kids cope during the pandemic
The pandemic and the resulting lockdown can be a confusing, even distressing time for children. Here’s advice on how to tackle it whatever their age.
Sometimes there are tears, other times tantrums, while often it’s a combination of the two. For many parents it’s been bewildering to see their usually sweet-tempered child having a meltdown, especially when it seems to have come from nowhere, as the pandemic goes on.
But it’s not surprising, experts say. If the pandemic is hard for adults, imagine how difficult it’s been for kids who are unable to manage or often even verbalise complex emotions.
Unexpected school closures, not being able to visit their grandparents or loved ones with comorbidities and not understanding why their parents are working from home – their whole world has been turned upside down, and it’s leading to serious breakdowns.
So, what can you do to help your child cope with this scary reality? We spoke to experts to help you tackle this tricky time.
A tantrum is not just a tantrum
Acknowledge that your kids may be battling emotionally, says Jasmin Kooverjee, a clinical psychologist based in the psychology department at Wits University.
“Children may become moodier, throw more tantrums, cry and become overwhelmed more than usual,” she says. “Remain patient and empathise with your child so they feel heard and acknowledged.”
Younger children especially rely on their parents to help them to understand their emotions, according to Lisa Saville Young, a clinical psychologist and associate professor at Rhodes University in Makhanda.
Try to be curious instead of judging their behaviour, she suggests. Be open and try to understand their actions because this leads to a better grasp of what they’re feeling – and can lead to less conflict in the home.
Be honest and direct
Children are always absorbing things happening around them, whether from the news or from hearing adults talk. So, you should absolutely not lie to them about Covid-19.
Talk in a calm, reassuring tone and explain that while life is strange right now, it won’t be like this forever.
Start by asking what your child understands about the situation. For example, “Lots of people are talking about coronavirus. Do you know what that is?” or, “You might have noticed Mommy is working from home. Do you know why?”
“It’s important to explain the pandemic in simple terms to your children, depending on their age and developmental level,” says Cape Town occupational therapist Nasreen Cariem. “By now, most children are aware of the virus, and they might be experiencing some anxiety over it.
“Toddlers won’t be aware of the virus, and they need their parents’ guidance in this time. But older children and teenagers need their parents to verbally address the issue because they’re better able to understand,” she says.
Visual aids – which you can get from several medical sources – can be handy when explaining the situation to them.
“It’s important to go through the process with them: how the virus is contracted, how contagion can be prevented and what the effects of the virus are.”
Put up signs and messages in the house to remind them to wash their hands and not touch their face, Cariem says.
“It’s important to be a role model and practice good hygiene – that way, your kids will follow your example. It’s also important to stay calm so the home is a tranquil haven amid a world that’s fallen into chaos.”
Children between 2 & 5
It’s especially difficult for younger kids to understand why their parents are working while at home – usually they’re home more over weekends, and it means family time and playing. This age group, says Kooverjee, may struggle more with tantrums and outbursts because they can’t voice their emotions.
“When parents notice this behaviour, rather than reacting in a punitive way, offer comfort and reassurance,” she says. “Let them express their feelings in non-verbal ways such as drawing a picture.”
Ask how they’re feeling and really listen to their answer. Tell them what you’re doing to make things better. For example, “I know you’re missing Granny. How about we video call her?”
Your child might want or need to talk while you’re working, but if you can’t, tell them you can’t listen then, but you will as soon as you can. For example, “I’m talking to my workmates on the computer right now, see? Can we talk after you’ve finished your puzzle?” But be sure to follow through otherwise the trust will be broken.
Stick to a routine. Waking up, brushing teeth, eating and going to bed at the same time helps give children a sense of normality.
Children between 6 & 10
Kids in this age group are able to express their feelings but may need help understanding that all emotions are acceptable, even scary ones, says Saville Young.
Make quality time for your child so you can pay attention without judgement, she advises.
Encourage children to entertain themselves so you’re able to work and have some time to yourself. “Sometimes this might mean letting them make a mess or have some screen time.”
You don’t need to be available to your children every waking hour. “Rather, when they do require attention, make it quality time.”
Following the three Rs is a way parents can help children cope if they feel overwhelmed, says Kooverjee.
Regulate: Help your child get to an appropriate emotional level. Go down to their level, hold them if they let you, stay calm and soft with body language that lets them know the space is safe. Help them to take deep breaths to slow their breathing and heart rate.
Relate: Use short sentences and let them know you understand what they’re going through. Say things such as, “I can see you’re frustrated. It must be hard not to see your friends right now.”
Reason: Once the child is calm, have a conversation about whether they understand their actions and feelings. Then ask what they need from you. Empathise and acknowledge what they’re going through.
Teenagers
“It’s easy to forget teenagers are still developing, particularly with regard to the ability to think through what they do before they do it. Have realistic expectations,” says Saville Young.
“Your teenager may be in an adult body, but their brains are still developing. Impulsivity and reactivity are likely. It’s important you remain calm and help them think through the thoughts and feelings behind their actions.”
It’s also important to make sure they watch the news and to communicate to them the importance of ensuring they get their information from reliable sources. That said, limit their access to Covid-19 news so it doesn’t become all-consuming or distressing.
Teens may look as if they want to be alone, but they also need quality time – as long as it’s not too overwhelming. “The key is to seek out time with them that doesn’t make them feel like they’re under a microscope,” Saville Young says. “Try to do something every day with your teenager that results in a positive interaction – cooking, baking or watching a TV series together.
“They’re more likely to seek you out to share their feelings if you have positive interactions with them during the day.”
EXTRA SOURCE: RAISINGCHILDREN.NET.AU

Feeling drained and anxious? Here are ways to destress
Whether you're working from home or you’re back at the office, it’s important to take time out to keep yourself feeling more relaxed and less stressed.
Due to the coronavirus pandemic persisting, it's understandable that you might be feeling exhausted and anxious during this time of uncertainty.
Here are five simple ways to help you destress and feel energised.
Get up earlier
This isn’t for everyone, but if you’re more of a morning person then start rising even earlier.
You’d be surprised at how much more you’ll accomplish before everyone else is awake. This way you’ll feel more in control of your day and less overwhelmed, whether you use the extra time for reading, getting in a workout, responding to emails or getting right to work.
Completing these tasks first thing in the morning allows you to focus on your to-do list sooner – which means you get done earlier and can fit in something that you enjoy, according to The Conversation.
Take a walk, even if it's for a few minutes
Exercise is one of the best stress relievers out there. But not everyone will take the time or have the motivation to commit to a strict workout plan.
Worry not! Fitting in a short 10-minute walk first thing in the morning, during a lunch break or after you’re done with your work can do wonders for your mental health. A short walk clears your head and boosts endorphins, which in turn reduces stress hormones.
If possible, go for a walk around your neighbourhood or anywhere where you feel relaxed.
Enjoy a balanced diet
Your mood is easily influenced by food. This is why you automatically reach for your comfort food when you feel down in the dumps or stressed out. Nonetheless, cookie dough for breakfast is never the best option for your health.
Healthy eating improves your energy, makes you more productive and improves your physical and mental health, according to Every Day Health.
“Microbiome health, or gut health, affects your mood, emotions and psychological health,” says Alice Figueroa, a nutritionist in New York City and founder of Alice in Foodieland.
Meditate
Take time out and just breathe. This practice of inward-focused thought, along with deep breathing, has been proved to reduce heart disease risk factors including high blood pressure, The Stylist reports.
Meditating methods include yoga and prayer, which are also effective in relaxing the mind and body.
This could even be done in just five minutes.
Get enough quality sleep
Sleep is an essential part of staying healthy and strong, and it can help you better handle stressful situations.
Remember, just because you’re in bed for eight hours doesn’t mean that you’re getting quality sleep. Make sure that you get restful and restorative sleep every night by having a cool, dark and quiet environment.
The Sleep Foundation recommends that adults get between seven to nine hours of sleep every night.
SOURCES: NIVEA.COM.AU, STYLIST.CO.UK, WEBMD.COM

How to manage stress during the pandemic
If there is anything the Covid-19 pandemic has taught us, it’s that every now and then something you have no control over will come along and throw you for a loop.
In 2020, a national survey conducted by pharmaceutical company Pharma Dynamics showed that 56% of South Africans experienced higher levels of emotional and psychological distress than they did before the coronavirus came along and ripped the carpet out from under our feet.
The results, released in October to coincide with Mental Health Awareness Month, revealed that 53% of the more than 1 200 polled respondents had either lost their job, had to take a pay-cut or were forced to close a business after lockdown began in March 2020.
The study also showed that 65% admitted to neglecting their health, 44% struggle to relax and 68% are worried about the impact of the pandemic on society and the economy.
It’s more important than ever for people to take their mental health into consideration, says Tamara Sosa, a Johannesburg-based counselling psychologist. “And we need to build mental resilience as we try to work out how to navigate our new day-to-day lives,” she adds.
The truth is you cannot inoculate yourself against stress, but you can find ways to calm the inner turbulence it causes. The answer, experts say, is to stop seeing stress as a negative and try to view it as an opportunity for personal growth.
You can do this by identifying your personal stressors, consciously deciding how you respond to them and managing the impact they have on you, says Sean Waters, a stress specialist practitioner and founder of Stress Less Clinic in Johannesburg.
Here’s how to go about it:
Recognise the problem
It’s not unusual to be so caught up in a stressful situation that you ignore how it’s making you feel. The first step is to acknowledge that the effect it’s having on you is problematic. “If you can say, ‘I recognise that I have a problem’, then like an addict that reaches out and says, ‘I need help’, you’re now at the point of realising something needs to be done. That’s a huge step,” Waters says.
Check your habitual response
We all respond to stress in our unique way. There are many things that influence how you deal with stress, says Leone Malan, a human physiology professor at North West University who specialises in stress responses in the brain and heart.
“These include your personality, your perception of the stressors as a challenge or a threat, previous experiences and your emotional and physical resources.”
Waters says recognising how your body and mind respond to stress takes honesty and self-reflection and once you identify this, you’ll be able to respond in a more purposeful way.
Keep track of yourself
Self-tracking is pivotal when you’re changing habitual behaviour patterns. Waters recommends tracking some key areas to get you started – your diet, sleep, exercise, productivity, relationships and finances. “I’d suggest doing this tracking exercise for a minimum of 14 days, but ideally up to 30 days,” he says.
Practise positivity
Rather than making you feel more in control, irrational thinking and catastrophising will make you feel more stress.
“Unfortunately, our brains love negativity,” Waters says. This is because our survival depends on identifying threats, so we’re hardwired to look for them.
Identify what you need to change and track it to foster good habits.
“Let’s say exercise comes up. Instead of telling yourself you don’t have time, say to yourself, ‘I need to find ways to exercise more regularly and part of that is finding a type of exercise that suits me’. Commit to a schedule and find a way to track it,” Waters says.
Let your brain breathe
Your brain needs a break sometimes. We run it through its paces daily, thinking up new ideas, planning or even learning something new.
Try some self-soothing activities to give your brain a rest. Self-soothing involves engaging your senses, so it could be hugging someone you live with, having a bath with aromatherapy oils or sitting by the ocean and watching the waves.
You can also give your brain a chance to breathe and energise by actively doing habitual actions in a non-dominant way, Waters says. “Simple things such as brushing your teeth or eating with the hand you don’t normally use will help to rewire your brain in a positive way.”
Learning to cope
As we continue to navigate through these uncertain times, learning to cope with the “new normal” is a skill you can teach yourself. Here are four things you can do to develop and cultivate that skill.
Take note of the story you’re telling yourself:
How and what you think plays a big part in how you feel. Telling yourself that stressful things sometimes happen will help you accept that change. “Mental resilience means noticing our own thoughts and unhooking them from non-constructive ones,” Sosa says.
Learn to let go of thoughts that leave you feeling overwhelmed or anxious and start telling yourself instead you’ll get through it.
Build your support network:
We’re social animals, so it’s no surprise that people with strong support networks and social ties are more likely to recover faster from traumatic events.
“One of the most important factors, if not the most important, is to have a squad, a group of individuals who you really care about and who will come to your aid no matter what,” says Steven Southwick, a professor of psychiatry at Yale University’s School of Medicine in the US and co-author of Resilience: The Science of Mastering Life’s Greatest Challenges.
Reach out to those around you. Personal interaction facilitates the release of the hormone oxytocin, which provides a buffer against stress by lowering the heart rate, counteracting cortisol, boosting fearlessness and promoting a feeling of connectivity and positivity.
Practice mindfulness:
Mindfulness has become a buzzword in recent times – and for a good reason. It’s about bringing your attention to what you’re experiencing in the present moment in a way that simply observes and doesn’t judge. “Mindfulness trains you to become an observer of your thoughts and emotions,” Southwick says.
Instead of viewing stress as something to get rid of, it could be used as a tool. Train your brain to perceive something stressful as a challenge instead of a threat.
Prioritise your wellbeing:
Exercise regularly and eat a well-balanced diet.




The devastating effects of long-haul Covid and how you can deal with them
Not everyone who gets the virus recovers quickly. Symptoms can plague you for months. What are the long-term effects?
When she was diagnosed with Covid-19 in May 2020, Stacey Smith* was surprised considering the precautions she’d taken.
But what surprised her even more was how long the symptoms lasted. While some went away reasonably quickly, other remained for months after her test came back positive.
“The symptoms I presented with at the start were fatigue, headaches, tummy issues, loss of smell, tight chest, shortness of breath, joint pain and brain fog,” Stacey (46) tells us.
She was also diagnosed with pneumonitis (inflammation of the lung tissue) as well as inflammation of the arteries in her lungs.
Most of Stacey’s symptoms cleared up after a few weeks, and her sense of smell returned after a few months. Yet, six months after being diagnosed with Covid, some symptoms remained – the most pronounced one being fatigue.
Stacey describes feeling as if the tiredness was in her bones, and she found short outings or trips to the doctor incredibly tiring.
Other persistent symptoms included joint pain, occasional brain fog and headaches. Her asthma, which had been stable since childhood, became problematic after her diagnosis, and she’s had to use her pump twice a day.
Stacey’s case isn’t unusual. While most people who’ve had Covid-19 recover completely within a few weeks, some continue to experience symptoms for months after their initial “recovery”. It can even happen to those who had a mild version of the disease, and the ongoing symptoms can be debilitating.
It’s informally known as “long Covid” and some people report “life-changing experiences that follow an initial infection that they managed at home, with symptoms becoming more severe over time”, according to a review by the UK’s National Institute for Health Research.
Lingering Covid-19 symptoms
Although Covid-19 is a disease that primarily affects the lungs, it’s become clear that it can damage other organs as well. The virus can cause significant cellular-level damage, says Dr Gregory Poland of the Mayo Clinic’s Vaccine Research Group, and this increases the risk of long-term health problems.
Long or long-haul Covid is “a multi-system disease”, says Professor Adrian Puren of South Africa’s National Institute for Communicable Diseases. What commonly happens is that symptoms arise in one physiological system, then subside only to arise in a different system, he says.
The most common symptoms include cough, low-grade fever and fatigue, Puren adds. “Other reported symptoms include shortness of breath, chest pain, headaches, neurocognitive difficulties, muscle pain and weakness, gastrointestinal upset, rashes, metabolic disruption (such as poor control of diabetes), thromboembolic conditions (blood clots) and depression and other mental-health conditions.”
Less common long-term symptoms include absence of smell, dry mouth and eyes, runny nose, red eyes, headache, absence of taste and issues involving the heart, says Professor Willem Hanekom, director of the Africa Health Research Institute.
Both those who’ve had mild and severe Covid-19 might have long-term effects, whether they have comorbidities or not, Hanekom says.
“These long-term effects aren’t caused by ongoing infection with the virus that causes Covid-19, but rather by inflammation – the body’s response to the infection – which is ongoing,” he adds.
Long-term symptoms include:
Heart damage: Scans taken months after recovery have shown lasting damage to the heart muscle, even in those who experienced only mild symptoms.
Lung damage: The type of pneumonia commonly associated with Covid-19 can damage the tiny air sacs (alveoli) in the lungs and the resulting scar tissue can lead to long-term breathing problems.
Brain damage: Covid-19 can cause strokes, seizures and Guillain-Barré syndrome, an autoimmune condition that causes temporary paralysis. It might also increase the risk of developing Parkinson’s and Alzheimer’s disease.
Blood clots: The disease can make blood cells more likely to clump together. Much of the heart damage caused by Covid-19 is believed to be due to small clots blocking tiny blood vessels in the heart muscle.
Blood-vessel problems: The disease can also weaken blood vessels, which can potentially lead to long-lasting problems with the liver and kidneys.
Fatigue: It’s been noted that many people who recovered from severe acute respiratory syndrome (Sars) have gone on to develop chronic fatigue syndrome, a complex disorder characterised by extreme fatigue that worsens with physical or mental activity. The Mayo Clinic says the same might be true for people who’ve had Covid-19.
How long do the symptoms last?
It’s difficult to predict long-term outcomes because Covid-19 is such a new disease, but research is ongoing, and scientists can draw expectations from similar diseases.
“Possible causes of the long-term symptoms include relapse or reinfection, inflammation and immune reactions,” Puren says.
“These have also been the case with other more severe coronavirus infections, including Sars and Middle East respiratory syndrome (Mers).
“Many patients recover spontaneously – if slowly – with holistic support, rest, symptomatic treatment and gradual increase in activity,” Puren says.
Hanekom adds that many infections have post-infectious inflammatory symptoms such as an ongoing cough after a mild viral chest infection. In most cases, these inflammatory symptoms eventually subside, which is what’s anticipated for Covid-19 too.
Tips for Covid long-haulers
Here’s what to do to aid recovery, according to the UK’s National Health Service:
Eating healthily: It’s vital for recovery so your body gets the energy, protein, vitamins and minerals it needs. Focus on fresh, nutrient-rich foods.
Get moving again: If you’ve been hospitalised or in bed for some time, your muscles will have weakened. Go slowly but do what you can to improve your fitness.
Reach out: Support from relatives and friends is vital. Those caring for or close to someone who’s had Covid-19 should find a balance between supporting them and encouraging them to get back on their feet as soon as possible.
Where to get help
There are several support groups you can reach out to.
Covid-19 Support Group South Africa: A private Facebook group aimed at providing emotional support and useful information on Covid-19.
Long Covid Support Group: A private Facebook group; exclusively for long-haulers and those caring for them.
Long Haul Covid Fighters: A private Facebook group for survivors recovering from Covid-19 who were diagnosed on or after 1 April 2020.
/r/COVID19Positive: A group on the discussion platform reddit.com where people who’ve tested positive can share their stories and experiences, answer questions and vent.
*Not her real name.
EXTRA SOURCES: MAYOCLINIC.ORG, MEDICALNEWSTODAY.COM, SCIENCEMAG.ORG
Are you wearing your mask incorrectly? And can your employer force you to go back to the office if you’re pregnant? We answer these questions and more.

Pregnant during the pandemic? Know your rights at work
We answer important questions about pregnancy, your job and Covid-19
There’s no definite scientific proof that pregnant women get sicker than others if they catch Covid-19. But it’s still a worrying time for those expecting a baby.
Can they be forced to return to the office? And can they still get maternity leave, even after having worked from home during lockdown? We answer three questions about pregnancy and your job.
I’m pregnant and nervous. Can my employer force me to return?
By law, your employer must ensure a safe working environment in which your health isn’t at risk. Many employers are making alternative plans for pregnant employees to minimise the risk of infection.
If you perform high-risk tasks, such as working with clients, you can ask that these interactions be minimised or that you’re given a separate workspace such as your own office.
Some employers are also organising alternative transport for pregnant women who usually use public transport. You can also request additional paid leave, but this will probably be on a quid pro quo basis – meaning you have to work those hours in at a later stage.
If alternative arrangements are made for you, such as adjusting your work activities or renting an office space for you, the cost shouldn’t be deducted from your salary.
If your pregnancy is at 28 weeks or more, you fall into the vulnerable category of employees, along with those with chronic conditions such as diabetes. It’s quite possible that your employer would prefer that you work from home.
You may refuse to return to work if you’re worried. But you can only do this if there’s a real risk of exposure to the coronavirus. If this is the case, you need to notify your employer or the company’s health and safety officer as swiftly as possible.
You’ll need to provide reasons for not returning to work so the employer is given a chance to solve the problem. In most circumstances your employer isn’t allowed to deduct from your salary if you decide not to return to the office due to safety concerns.
What about maternity leave during a pandemic and lockdown?
The same rules apply as under normal circumstances, so you’re allowed maternity leave during lockdown.
The Basic Conditions of Employment Act allows for at least four months’ concurrent maternity leave. It can be taken from four weeks before the due date, or a date your doctor recommends. You’re not allowed to return to work sooner than six weeks after your baby’s birth unless your doctor approves it.
Your employer isn’t legally obligated to keep paying you while you’re on maternity leave – unless your contract states that you must be paid partially or in full, or it’s part of the company’s policy to continue paying a salary during maternity leave. If you’re not receiving your full salary during your maternity leave, you can claim maternity benefits from the Unemployment Insurance Fund (UIF) – provided you contributed to it.
Your employer’s human resources department can tell you if you contributed to UIF and provide you with the correct paperwork.
Can a pregnant employee be laid off?
A pregnant employee may not be discriminated against, which means you can’t be laid off because you’re pregnant. But pregnant employees may be laid off or retrenched for operational reasons, for example if the overall business is suffering due to the struggling economy.
Your employer must be able to prove that there’s a valid reason for the retrenchment and that it was inevitable. They must then follow the correct retrenchment process. Included in this is suggesting alternatives, such as only having you work half-day instead of full days to save costs.
You may also not be summarily discharged. There needs to be a notice period, which will depend on how long you’ve worked there. You must be paid during the notice period, even if you’re not required to work.
If you’re retrenched, you’re entitled to the following:
· SA retrenchment package equal to at least one week’s pay for every full year of service.
· Your salary up to and including your last working day.
· All payments due to you, such as commission and overtime as well as accrued leave.
· If you’re a member of a company retirement fund, that must also be paid out in accordance with the retirement fund’s rules.
· Depending on your contract, you may be eligible for a pro rata bonus.
If you have reason to believe you were unfairly discharged, you can approach the Commission for Conciliation, Mediation and Arbitration (CCMA) for advice.
Tip: The same maternity benefits that apply to biological parents also apply to adoptive parents during the pandemic and lockdown.
Get help here:
· UIF: www.labour.gov.za
· CCMA: www.ccma.org.za or call 0861-161-616


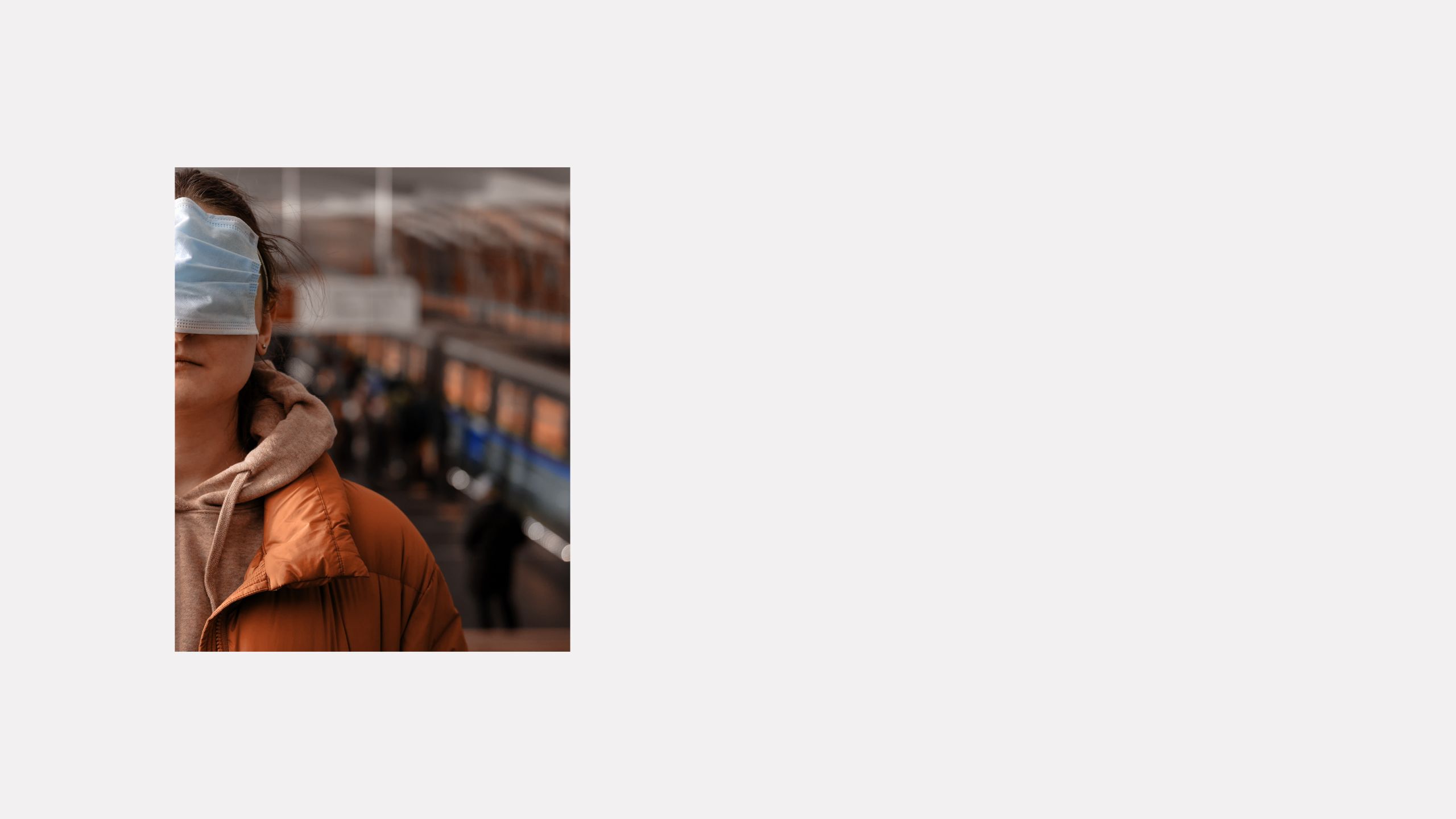
There are 6 ways you could be wearing your mask incorrectly – see if you're doing it wrong
The mask can be a mighty weapon in the fight against Covid-19 … if you wear it properly. Experts are unanimous: wearing a mask is one of the most basic ways you can help fight the virus that’s claimed the lives of more than four million people around the world.
Yet so many don’t wear their masks, or they wear it in a way that doesn’t offer the right kind of protection.
Yes, masks can be irritating – especially on hot days. That’s why so many of us have become increasingly creative in the ways we choose to wear them. But doing so increases our risk of getting sick.
Make sure you’re not falling into any of these mask traps and see what you can do to make it more comfortable.
1. The nose tickler

This is one of the most common. Exposing your nose may make it easier to breathe – but it also means viruses can get up your nostrils. You might as well not be wearing a mask.
2. The dangler

Masks get stuffy, spectacles get foggy and sometimes you just want to breathe in fresh air, so many people tend to dangle their mask from one ear as they walk from store to store. But your mask could fall to the floor and pick up germs. And if your hands are dirty and you’re taking off and putting it back on with your dirty hands, you could be transferring germs.
3. The straw door

A favourite of foodies. Many diners want to err on the side of caution when they’re eating, so they make an incision in their mask, either as a hole through which to sip a straw or by making a bigger gash in the mask to be able to take mouthfuls of food.
This makes the mask less efficient. “If you’ve cut a big hole in it, it’s not doing any good because you’re just breathing the droplets out,” Professor Catherine Noakes, airborne disease transmission expert at the University of Leeds in the UK, told The Guardian.
A hole for a straw isn’t as bad. “If you had a tiny slit, just enough to pass a straw through, that’s likely to be quite a lot better than not having a mask on at all,” she says.
4. The mouth flasher

Some people cover only their noses to allow for lip-reading. This exposes other people who can catch airborne droplets from you. It also doesn’t protect you if you breathe in through your mouth.
5. The hammock

This is another popular trend many are guilty of: wearing the mask below the chin. It’s as good as not wearing a mask. It increases the risk of germs spreading over your face and neck as you adjust the mask up and down over your chin.
6. The visor

A visor keeps big droplets from your eyes and mouth but on its own it won’t protect against smaller airborne droplets. Combine it with a mask – that way a visor provides extra protection around the eye area while the mask covers your mouth and nose.
Help! Complaints and questions
Wearing a mask hurts my ears:
Choose a cotton mask with cotton ear ties that fasten at the back of your head rather than one with an elastic ear loop. Or attach your ear loops to buttons sewn onto the side of a headband or hat. You could try an ear-saver clip that’s positioned at the back of the head and is used to hold elastic ear loops.
How often should I wash my cloth mask?
Masks need to be hand-washed, advises Nkosinathi Lowan, founder of Health Zone Pharmacy and Clinic. Ideally, you should change a cloth mask after three hours of use. If you have a washing machine, you can use that, but in general you just need water and soap. Wash it for a few minutes, hang it to dry and then destroy any lingering germs with a hot iron.
Can I reuse a disposable mask?
Yes. When you remove your mask, touch only the ear straps, avoiding the surface of the mask as much as possible. That’s where virus particles may have gathered, advises Dr Lucian Davis, an epidemiologist at the Yale School of Public Health in the USA.
Once the mask is safely removed, put it in a clean receptacle.
Jade Flinn, nurse educator at Johns Hopkins Medicine in Baltimore, USA, says she puts her mask in a paper bag – this allows good ventilation – for the mask to air out for a few days. If a mask is soiled or torn, discard it.
My glasses fog up when I wear a mask:
Look for a mask with a metal wire sewn in that goes over the bridge of your nose. Then you can pinch the top of your mask so that it fits the shape of your nose, says Dr Sidney Gicheru, clinical spokesperson for the American Academy of Ophthalmology in Dallas in the US. Tighten the sides of your mask by adjusting the straps so it fits snugly.
Another option is to put a plaster on the bridge of your nose to close the gap between your nose and your mask. Many optometrists now offer sprays that can prevent fogging for a few hours.
My mask keeps slipping down:
It’s important not to touch your mask because of the risk of contamination.
Make sure your mask fits you correctly before you leave home. When you put your mask on, you should notice it moving in and out as you breathe, says William Schaffner, a professor of medicine at the Vanderbilt University School of Medicine in Tennessee in the US. If it doesn’t, you need to tighten it. Adjust the ear loops and tie a knot so the mask fits snugly against your face and there are no gaps at the sides or top.
Or put a plaster on the bridge of your nose to close the gap between your mask and nose. Refrain from fidgeting with the mask once you’ve put it on, advises Lowan. Carry sanitiser so if you do touch the mask to fix its positioning, you can sanitise your hands afterwards.
Masks are too small for my head:
Try tying a shoelace or piece of string to each ear loop. After putting on your mask, tie the extended strings together at the back of your head.
From conspiracy theories to concerns about safety, there is a lot of misinformation on the vaccines. We spoke to experts to get the facts and find out how the vaccines will protect you against Covid-19.

Covid-19 antibodies: How they work and how safe they make us against the new variant
If you’ve had Covid-19, you’ll have developed antibodies that are meant to protect you. But how do they work?
It’s one of the words buzzing around out there in this strange new world of ours, where medical terms trip off our tongues with an ease we couldn’t have imagined before.
This one is antibodies: a word seen by some as representing a get-out-of-jail free card, an “immunisation passport” of sorts. Because once you’ve had a virus, antibodies are what you develop – little soldiers marching about in your body, batting off infection for a while.
And it’s a comfort to people who’ve had Covid-19: you’ve been there, done that and got the antibodies to prove it.
But hang on a second. What about the new variant that’s caused so much havoc here and abroad – do antibodies from a previous Covid-19 infection still protect you? And how do we go about finding out if we have antibodies anyway? How do they work exactly and just how safe do they make us?
We went in search of the answers.
What are antibodies?
Antibodies are proteins called immunoglobulins or Igs which are produced by the body to defend against an infection, explains Dr Vidya Lalloo, emergency medicine specialist at Steve Biko Academic Hospital.
“There are five classes of antibodies but when we talk about immunity, we usually refer to IgM and IgG antibodies.”
Immunoglobulin M (IgM)
This is the first antibody produced when we contract an infection. Production starts quickly, within three to 10 days of contracting an infection, Lalloo says, but its production wanes within a few weeks.
Immunoglobulin G (IgG)
This antibody is usually produced later – around seven to 21 days after infection – but in usual circumstances lasts much longer than IgM, sometimes for months or even years, Lalloo says.
About 70-80% of immunoglobulins in the blood are IgG and they form the basis of long-term immunity.
When you have an infection (other than Covid-19), the body builds a catalogue of IgG antibodies that can be rapidly reproduced when exposed to the same infection again.
Usually, in people with normal immune systems, enough IgG is produced to prevent reinfection.
However, Covid-19 antibodies seem to give only limited protection against reinfection. “These antibodies wane quickly too, and, in some patients, they may be undetectable two to three months after infection,” Dr Howard Newman says.
How do I get an antibody test?
It’s pretty easy to get one in SA. Most pharmacies, including Clicks and Dis-Chem, offer rapid-result tests at affordable prices. Major pathology laboratories – including Ampath, PathCare and Lancet – offer more comprehensive tests.
How it works:
In a pharmacy
A few droplets of blood from a finger prick are needed for a lateral-flow test strip (similar to home pregnancy strip tests) where a line becomes visible if antibodies are present. Some of these rapid tests can measure both IgG and IgM, Newman says.
But because not all brands of lateral flow tests pick up both IgG and IgM, they might not be as accurate as a test done in a lab.
Pros: Results are available within 15 to 30 minutes. And at between R130 and R150, the test is relatively affordable.
Cons: Rapid antibody tests aren’t perfect and can produce false positives.
In a lab
Enough blood must be drawn into a tube for what’s called a serology test. Lab tests are far more sophisticated: technicians use a process that measures the binding of antibodies and proteins called an enzyme-linked immunosorbent assay (Elisa), which produces the most sensitive results.
Pros: False positives are rare.
Cons: Results take between 24 and 48 hours to be released. A lab test costs more – between R225 and R274, depending which lab you go to.
What are the benefits?
A Covid-19 antibody test is particularly helpful in identifying recent past infections, including in asymptomatic people, says Dr Lee-Anne Godinho, specialist physician at Mediclinic Midstream Hospital near Pretoria.
In the medical world, antibody tests are beneficial in three areas: diagnostics, research and screening.
Diagnostics
· When a Covid-19 test – known as a polymerase chain reaction (PCR) test – is negative but a patient has had symptoms of Covid, they may have tested too late. A positive antibody test result can tell whether the patient had contracted the virus.
· When a patient has symptoms similar to post-Covid complications but didn’t have a PCR test, an antibody test might help diagnosis.
· If there’s a discrepancy in PCR test results, a positive antibody test result would confirm the patient has had a recent coronavirus infection.
Research
· To identify donors for convalescent plasma therapy. “Sometimes the blood from people who’ve recovered from an illness can be used to make products that could potentially treat others with that same infection,” Newman says. Plasma therapy for Covid-19 is still in the study phase.
· To check that vaccines are successfully producing enough antibodies in those who have been inoculated.
· To study the prevalence of the disease in a population. Positive antibody test results can show outbreak numbers, identify hotspots and help monitor certain high-risk groups (such as in nursing homes, hospitals and prisons).
Screening
· For asymptomatic people in high-risk professions who have had Covid.
· For asymptomatic individuals in quarantine facilities.
· For asymptomatic patients before admission to hospital for elective procedures.
If I’ve had Covid-19, am I still at risk?
You have some immunity, Godinho says, “but we don’t know how much protection is provided or exactly how long it will last”.
How long immunity lasts is one of the big questions in the pandemic. Research is still ongoing.
What about the new variant?
Everyone should consider themselves at risk, the experts say. In January 2021, The National Institute for Communicable Diseases of SA issued sobering findings. “Mutations have allowed the virus to become resistant to antibodies,” the institute said in a statement.
“Blood samples from half the people we tested [who’d previously had Covid-19] showed all neutralising activity was lost.”
A study in the US found that 10% of Marines who’d had Covid-19 and tested negative repeatedly afterwards were infected again by a new variant.
“Previous infections do not give you a free pass,” says Dr Stuart Sealfon of the Icahn School of Medicine at Mount Sinai, New York. “A substantial risk of reinfection remains.”
Lalloo says it’s vital no one lets down their guard. “We’d hoped we would have immunity to the new variant but unfortunately this is not always the case. I personally know five healthcare workers who’d had Covid and got it again in the second wave.”
The refrain remains the same: wear masks, sanitise, keep your distance. There’s no get-out-of-jail card with this thing.
EXTRA SOURCES: ASSOCIATED PRESS, BRITANNICA.COM, CDC.GOV, MERCKMANUALS.COM, NICD.CO.ZA, SCIENCEALERT.COM, THE SCIENTIST
Facts vs fiction: Everything you need to know about vaccines and their safety
It's the world’s best hope of beating a virus that killed more than four million people, infected more than 200 million and brought mayhem and misery to a shell-shocked planet. Yet many have indicated they won’t accept the vaccine against Covid-19.
Fears abound: it was developed too fast. It could make me sick. Then there are the conspiracy theories – including one that a microchip could be inserted in your body with the jab that will allow Microsoft founder Bill Gates to track you.
It’s simply not true, of course – but authorities face an uphill battle getting people to believe the vaccine is safe.
In early 2021, before the vaccine was available in South Africa, an Ipsos study found that only about half (53%) of South Africans said they would get the vaccine.
And according to an Afrobarometer survey that the Institute for Justice and Reconciliation did amongst 1 600 South Africans in May and June, 42% of South Africans aren’t willing to the get the vaccine.
All the misinformation out there is fuelling the fear, says Professor Rose Burnett, head of the South African Vaccination and Immunisation Centre in the Department of Virology at Sefako Makgatho Health Sciences University in Pretoria North.
“Indiscriminate use of social media has made misleading information and conspiracy theories about Covid-19 go viral,” she adds. “The public is overwhelmed by anxiety and uncertainty and don’t know who to trust.”
The truth is without vaccines, diseases such as smallpox and polio would kill and affect millions. Measles, mumps and rubella would still be major illnesses.
And without a vaccine to combat Covid-19, it will be years before the world is anywhere near a semblance of normality. Here’s more about this lifesaving jab.
How do vaccines work?
They contain weakened or inactive parts of a germ that’s introduced into your body, usually by an injection. Your immune system reacts to the vaccine by making antibodies. The antibodies destroy the weakened vaccine germs just as they would the disease itself.
They stay in your body, waking up to give you instant immunity if you are exposed to the real germ.
Simply put, vaccines work by exposing you to a safe version of a disease before you get exposed to the real disease.
Are they safe?
Yes, Professor Burnett says. “Vaccines are subjected to rigorous safety testing and will only be released onto the market if they have been found to be safe and effective.”
Before being administered to the public, a vaccine is tested on animals, then on groups of humans. The vaccine is subjected to ongoing studies to monitor any potential side effects.
We now have vaccines to prevent more than 20 life-threatening diseases, enabling people to live longer, healthier lives. Immunisation currently prevents two to three million deaths every year from conditions such as diphtheria, flu and measles.
The growing anti-vaxxer movement has led to the return of measles to some countries in the northern hemisphere where it had been eradicated for years, says Dr Albie de Frey, an honorary lecturer in travel medicine at the University of the Witwatersrand.
What about the speed of the Covid-19 vaccine development?
There’s no need to worry, says Dr Nokukhanya Msomi, head of virology at the School of Laboratory Medicine and Medical Sciences at UKZN and the National Health Laboratory Service.
Advanced technology over the years has made the fast production of vaccines possible. “There may be short-term, mild vaccine reactions that resolve without complication or injury, but studies show the Covid-19 vaccines are safe.”
Usually, vaccines take around 10 years to develop, but thanks to advances in genomic sequencing, researchers successfully uncovered the viral sequence of this disease in January 2020 – about 10 days after the first reported cases in Wuhan, China.
But this doesn’t mean the vaccine was a “rushed job”. There have been such major advances in the science of vaccine development over the years that researchers were able to refer to this to develop the Covid-19 vaccine.
Specific technology that was used for the development of this vaccine has been researched for some time, which means it could now be created faster than ever.
So, while the jab may seem to have reached the market frighteningly quickly, scientists actually used information they have been gleaning for years to develop the vaccine.
“This speed of the development of this vaccine challenges our whole paradigm of what is possible in vaccine development,” says Natalie Dean, a biostatistician at the University of Florida in the US.
“It’s tempting to hope other vaccines might now be made on a comparable timescale against diseases like tuberculosis and malaria that kill millions of people a year.”
EXTRA SOURCES: DAILYMAVERICK.COM, TIMESLIVE.COM, WHO.INT
Covid-19 variants and vaccines – all your burning questions answered
We asked the experts about the Covid-19 variants and how vaccines will protect you against them.
The development of the Covid-19 vaccine was a light at the end of a very dark tunnel – until new variants of the virus started rearing their ugly heads.
What are the different variants? And will the vaccines currently being used in SA protect you from them?
We speak to experts to answer all your burning questions.
The variants
Alpha, Beta, Delta – just how many variants are there?
To date several SARS-CoV-2 variants have been documented. According to Professor Hannelie Meyer, the head of the South African Vaccination and Immunisation Centre (SAVIC) at Sefako Makgatho Health Sciences University, not all variants persist as some disappear soon after they emerge.
That’s why the World Health Organisation (WHO) categorises all documented variants as either “variants of interest” or “variants of concern”.
It’s the variants of concern we need to look at as there is clear evidence of its significant public health risk, Meyer says.
Earlier this year, the WHO identified four variants of concern around the globe: Alpha, identified in the UK; Beta, found in SA; Gamma, first detected in Japan and Delta, identified in India.
Delta became the latest variant of concern because it was rapidly becoming dominant in many countries across the world – including SA, Meyer explains.
As South Africa struggled to cope with the spread of the Delta variant, the Lambda strain started to appear. According to a report published by the KwaZulu-Natal Research Innovation and Sequencing Platform, the Lambda variant started spreading through South America in June 2021.
By 14 June, WHO declared it a “variant of interest” after Lambda was found in 31 countries, including Chile, Argentina, Ecuador and Australia.
Also referred to as C.37, the Lambda variant accounts for about 81% of the cases reported in South America.
“At this stage it’s not a problem in South Africa yet,” says Dr Angelique Coetzee, chairperson of the South African Medical Association.
Are all symptoms the same?
Since the start of the pandemic people have been educated to look for symptoms associated with the virus. These include dry cough, fever, loss of taste and smell, chest pain or difficulty breathing.
However, Coetzee says it’s difficult to clearly outline the symptoms of the Alpha variant.
“We don’t have that information as it’s not as fast spreading in SA,” she says.
With the Beta variant – which was the dominant variant until recently – symptoms include a sore throat, the loss of taste and smell, high temperature and body aches and pains.
Research on the symptoms of the Delta variant is still ongoing. According to Meyer, it seems as though the early onset symptoms of infection is very similar to those of the common cold.
“This includes nasal congestion or ‘sniffles’, scratchy, itchy or sore throat, mild headache and feeling tired,” she says.
These symptoms might be brushed off as a cold while you might have Covid-19.
Why is the delta variant so contagious?
Labelled by WHO as the “fastest and fittest” variant, the Delta variant is 60% more contagious than others. “Preliminary data estimates it is 30 to 60% more transmissible than the Beta variant,” Meyer says.
Being so highly transmissible, it’s spreading fast among the unvaccinated population.
According to Ravindra Gupta, Professor of Clinical Microbiology at the Cambridge Institute for Therapeutic Immunology and Infectious Diseases, scientists consider two components when they look at the transmissibility of any virus.
First, they study how the virus can replicate faster and make more infectious variants, but there is also an “antibody-escape component” that looks at how the virus mutates and avoids some of our antibodies.
This is why people who were previously infected with the Beta variant may not be immune to the Delta variant and could be susceptible to reinfection with the Delta variant, Meyer says.
How should you treat it?
With the symptoms of the Delta variant mimicking that of a common cold, the danger is people might ignore it and will therefore not isolate or test for Covid-19.
Most patients have a mild infection, particularly those in the young and healthy age group. “We still need evidence from South Africa but early evidence from the UK suggests there is an increased risk of hospitalisation within 14 days of testing positive for Covid-19 compared to the Alpha variant,” Meyer says.
While there’s no concrete evidence that the Delta variant will make you sicker than the others, it’s still important to treat the symptoms and take the necessary precautions as if you have Covid-19, says internationally renowned virologist and head of the ministerial advisory committee (MAC) on Covid-19 Professor Barry Schoub.
“If you’ve been in contact with someone who is positive, and you show any symptoms three to five days later you should get tested,” he advises.
When will it all end?
Experts suspect the virus is here to stay because just as they start to get a grip on it, the virus keeps surprising them with new mutations. “The virus will always be there,” Schoub says.
“But I think eventually science will conquer the variants.”
To do this, scientists need to make sure the virus doesn’t cause so much severe disease. “If there are enough people who are immune to the virus either from being infected or from the vaccine then it will stop circulating. Hopefully, it will eventually be a minor disease.”
As experts continue to learn about the virus and its variants, they will also learn how better to manage it over time, he adds.
The vaccines
How effective are the vaccines in SA against the variants?
The good news, Meyer says, is that the Covid-19 vaccines South Africa is rolling out does protect against developing severe disease, hospitalisation and death due to the Delta variant.
While there’s no clinical-trial data on the effectiveness of the Johnson & Johnson vaccine against the Delta variant in South Africa yet, she says laboratory studies suggest that the vaccine may be even more effective against the Delta than the Beta.
The J&J vaccine, which is given as a single shot, provides an estimated 64% protection against moderate to severe disease and 82% protection against critical Covid-19.
“Further good news is that data also suggests the vaccine works effectively up to at least eight months post-vaccination, which means a booster dose isn’t necessary at this stage.”
Based on data from the UK, the Pfizer vaccine, which is given in two doses, has shown high levels of protection against hospitalisation with the Delta variant after the second dose.
Are other vaccines being considered?
The South African Health Products Regulatory Authority (Sahpra) has provided an emergency use authorisation for the CoronaVac Covid-19 vaccine, manufactured by Sinovac Life Sciences Co in China.
However, associate professor Kenneth Mak from Singapore says there’s little data on the effectiveness of the Sinovac vaccine against the Delta variant.
Because it takes a very long time to register medicines in SA, Sahpra will not register the vaccine unless they have sufficient data on it.
There are also conditions attached to the emergency use of the CoronaVac Covid-19 vaccine. “The applicant has to periodically provide vaccine safety reports and results of ongoing studies before it can be approved for use or in this case emergency use,” Meyer says.
Meanwhile, Professor Rose Burnett from SAVIC says Sahpra is busy with a “rolling review” of the application for the Sputnik V vaccine made in Russia.
This means Sahpra will review the company’s data on a continuous basis until sufficient evidence on efficacy and safety has been provided. “National regulators can only evaluate an application that has been submitted by a locally licensed applicant,” she says.
Since Sahpra hasn’t received any applications for the registration of the vaccines manufactured by Moderna and Novavax, these vaccines cannot be considered for use in SA.
Can you choose your vaccine?
You don’t have a choice of vaccines as government selects which vaccinations are sent to vaccination sites around the country.
Meyer says the various vaccines are being equally distributed across the provinces. “The government considers various factors in distributing vaccines, including vaccine availability and logistics. For example, if it's a mobile clinic vaccination site, then having the single dose J&J vaccine is easier to administer," she says.
"As more vaccines become available, the options available to the public in a specific area are likely to increase."
The J&J vaccine is being used mainly for teachers, while the Pfizer vaccine is available at all the other sites.
If for example you have an allergy or contraindication on the specific vaccine offered at the site you are attending, you'll be referred by the vaccinator to another site where the alternative vaccine is available, she says.
"But if you don't have a specific allergy or contraindication, since all vaccines are more or less the same in terms of efficacy and safety, I recommend you get the vaccine that's available to you.”
Different vaccines work in slightly different ways, but Burnett says all of them basically train your immune system to identify and neutralise disease-causing micro-organisms without exposing you to the actual micro-organism.
“For example, the Covid-19 vaccines available in South Africa use the spike protein of SARS-CoV-2 to train the immune system. So, when you get vaccinated, your body develops an immune response against the spike protein of the SARS-CoV-2 virus,” she explains.
This means that when you are exposed to SARS-CoV-2, your body already has antibodies and immune cells. These allow you to fight the virus before it can multiply, establish disease, and make you sick.
While the vaccine can’t stop the virus from entering your body the great advantage is that you will not develop severe disease because your immune system has been trained and will clear the virus from your body before it can establish disease.
Meyer says vaccinations are the only way to safely bring our country closer to reaching population immunity. “The Covid-19 vaccines we are using in South Africa have been shown to be highly effective at preventing severe Covid-19 disease and death from Covid-19,” she says.
According to the health department’s Covid-19 dashboard, SA surpassed the 10 million vaccinations mark on 19 August.
However, at the start of August, it seemed as if the country's vaccine drive lost momentum as the number of daily vaccines given dropped, according to Dr Nicholas Crisp, deputy-director in the Health Department.
There have also been reports of batches of vaccines being thrown away at the end of the day because they don’t “keep”.
There will always be a certain percentage of vaccine wastage, says Meyer.
Vaccines are based on different technologies and have different properties, which is why each vaccine has its own storage requirements. The period it can be stored at a certain temperature also differs from vaccine to vaccine. “Vaccines exposed to undesired temperature ranges will result in a loss of potency and can also result in adverse events following immunisation,” she says.
Should there be any deviations from the storage requirements, vaccines must be discarded for patient safety.
To avoid wastage, many vaccination sites now allow walk-ins. Government has also opened up vaccinations for over 18s earlier than they initially planned.
To register on the department of health’s Electronic Vaccination Data System all you need is access to the internet, your ID number or passport, contact information and your work or home address.
You can also register for a vaccine appointment at your local pharmacy if you are far from the site government allocates to you.
Meyer says there will be no vaccine wastage if you go to a different place instead of your registered site because the system will pick up your ID number. Walk-ins are allowed in case you miss your appointment.
*For more information on the EVDS registration and the Covid-19 Public Hotline, go to sacoronavirus.co.za.
EXTRA SOURCES: BUSINESSTECH.CO.ZA, DAILYMAIL.CO.UK, DAILYMAVERICK.CO.ZA, JNJ.COM, KRISP.ORG.ZA, NEWS24.COM, NGS-SA.ORG, NICD.AC.ZA, NYTIMES.COM, TIMESLIVE.COM